Cornea, IOL
Knowing Iris Repair: Aniridia
This next part in our series helps surgeons feel more prepared for aniridia cases.
Soosan Jacob
Published: Monday, June 3, 2024
Aniridia refers to the absence of iris tissue. It can be congenital or acquired and can be partial or total. Acquired causes include post-traumatic and iatrogenic (post-surgery).
Congenital aniridia is associated with a mutation in the PAX6 gene on chromosome 11p13. It is inherited most commonly as an autosomal dominant disease (85%), but also sometimes as autosomal recessive or as a de novo mutation (sporadic -13%).
Sporadic aniridia may be associated with Wilms tumour, genitourinary abnormalities, and growth retardation (WAGR syndrome). Wilms tumour is seen in one-third of sporadic cases since the deletion of the short arm of chromosome 11 may involve both the PAX6 gene and the adjacent Wilms tumour gene. Autosomal recessive aniridia is called Gillespie syndrome and has aniridia, cerebellar ataxia, and mental retardation as associations.
Congenital cases are not truly aniridic in the strict sense, as a small hypoplastic iris is often visible on gonioscopy. This peripheral stump can result in peripheral anterior synechiae and angle closure glaucoma by the second decade. Other associated ocular abnormalities include myopia, limbal stem cell deficiency, corneal pannus, microcornea, microspherophakia, cataract, ectopia lentis, foveal and optic disc hypoplasia, coloboma, nystagmus, strabismus, and amblyopia. Evaluation of family members and regular ultrasound for ruling out Wilms tumour is required in sporadic cases. Genetic evaluation may also be useful.
Traumatic and iatrogenic aniridia
Traumatic aniridia may occur following a blunt or penetrating injury where a part of or the entire iris is lost or has to be excised during reconstruction.
Iatrogenic aniridia refers to partial or complete loss of the iris during a surgical procedure. This may be intentional—e.g., a large sector iridectomy during a previous surgery—or accidental, such as inadvertent iris avulsion during phacoemulsification/cortex aspiration or nucleus extraction in manual small incision cataract surgery.
Congenital aniridia management
Patients with congenital aniridia should receive amblyopia therapy and treatment for strabismus. Coloured contact lenses or tinted glasses can help decrease photophobia and improve vision. Prophylactic goniotomy may be of benefit in preventing glaucoma. The onset of glaucoma should routinely be looked for, and surgery is often required for intraocular pressure control, with maximal success rates given by glaucoma drainage devices. Co-existing cataract and/or ectopia lentis may necessitate surgery if visually significant.
Aniridia IOLs and iris prostheses are available and will be discussed in the next episode of this series. Depending on the severity, aniridia-associated keratopathy may need treatment ranging from just preservative-free artificial tears to simple limbal epithelial transplantation with or without keratoplasty. Graft failures are common, however. Prognosis for congenital aniridia is poor due to the frequently associated ocular comorbidities.
Partial aniridia secondary to trauma or surgery
Large sector iridectomies may seem daunting to correct but can be tackled efficiently in many cases. Microforceps are introduced through a paracentesis, and the residual stump of the iris drawn in to see the actual available tissue, which is often more than what is initially visible because of the tendency for the cut ends of the iris to retract. In addition, the cut ends may fibrose and incarcerate into peripheral anterior synechiae (PAS)—often possible to release by careful blunt dissection from the overlying stroma, taking care not to tear the iris.
The risk of creating a Descemet’s detachment during synechiolysis decreases by pushing the iris away from the cornea rather than pulling it towards the anterior chamber (AC). A microscissor can be useful to cut the corneal attachment of the PAS. Some bleeding may occur during these manoeuvres, and continuous infusion through an AC maintainer serves to tamponade and arrest bleeding. This can be aided by withdrawing instruments temporarily and increasing infusion pressure. Alternately, all manoeuvres may also be done with viscoelastic filling the AC.
Once the iris stumps on either side are released, the microforceps gently stretch the two ends towards the centre to see how much mobility can be obtained towards the opposite stump and the intended final position of the pupil. If impossible to repair, iris prosthetic devices may be used.
If apposition is possible, a combination of several techniques continues iris repair. Care should be taken to use gentle, controlled manoeuvres to prevent iris tearing, iridodialysis, haemorrhage, and other complications.
Single-pass, four-throw (SFT) pupilloplasty
An SFT technique brings the two edges of the iris stroma together. Decreased tension on the iris leaflets can be attempted, released by gentle and careful tugging on the iris roots to release any small synechiae in the angles. Multiple SFT passes taken adjacent to each other approximate the iris leaflets as much as possible without causing cheese-wiring or iris stromal holes.
This initial part of the repair results in the two iris leaflets coming together in an iridodialysis-type configuration.
Hang-back technique
The next part of the repair therefore addresses the gap present between the distal arc of the repaired iris and the scleral wall. The motility of the repaired iris towards the scleral wall and the displacement of the pupil on attempted apposition of the iris to the scleral wall are assessed both visually and by using microforceps to gently manipulate the iris.
In case the iris is mobile—but the pupil gets displaced on the apposing iris base to sclera—a trocar-assisted hang-back technique may be performed using a double-armed 10-0 or 9-0 polypropylene suture with long, thin needles on both ends. The iris is ‘hung back’ in a non-appositional manner from the scleral wall using the prolene suture, allowing the pupil to remain in the desired location. For a detailed description of this technique, see part three of this series on iris repair.
Classical iridodialysis repair
In case the iris is mobile enough to appose against the scleral wall without displacing the pupil being displaced, any one of the various iridodialysis repair techniques is acceptable.
Pupillary relocation
If the pupil is pulled to the side of scleral fixation, it can be recentred using the vitrector or microscissors to enlarge the pupil in the desired direction. If this enlarges the pupil too much, an additional SFT on the iridodialysis side (provided iris tissue allows) makes it small again. Mid-stromal iridodiathermy on the side to which the iris needs to be moved using the endodiathermy probe with just sufficient power to cause mild iris stromal contraction can also help relocate the pupil.
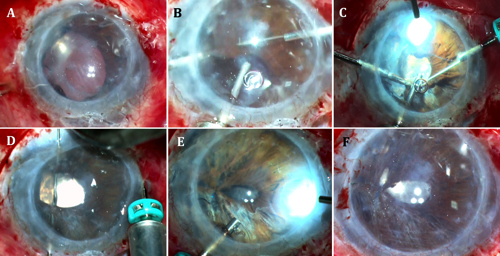
An alternate repair method is to first sclerally fixate the stumps of the iris, align them towards each other, close the gap using an SFT suture, then centre the pupil (see Figure).
Dr Soosan Jacob is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India, and can be reached at dr_soosanj@hotmail.com.
Tags: cornea, IOL, iris repair, Soosan Jacob, Jacob, series, aniridia, congenital aniridia, sporatic aniridia, hang-back technique, single-pass four-throw pupilloplasty, iridodialysis repair, pupillary relocation
Latest Articles
Going Beyond Cataract Camps
ESCRS expanding treatment opportunities in underserved areas.
Bridging the Gap Between Local and Global
New training programmes seek to reach hard-to-reach areas to meet growing patient needs.
2024 Congress Draws Global Audience, Strengthens Ties
Refractive EDOF with the Benefits of Monofocal
PureSee IOL studies indicate high patient satisfaction.
Making the Right IOL Decisions
Use of presbyopia-correcting lenses in post-corneal refractive surgery patients requires attention to multiple considerations.
Training to Target Global Cataract Blindness
Non-profit organisations look to innovative, scalable virtual reality training systems.
ESCRS Refractive Surgery Guidelines a Work in Progress
Challenges involve keeping up to date on current treatments.
Stabilising with PACE-CXL
Performed with advanced technologies, PACE-CXL procedure stops ectatic progression and improves vision.
Closing the Mentorship Distance
Addressing a need in underserved regions, distance surgical mentorship offers a viable strategy with multiple benefits.